



Published on Sep 12, 2023
Angina pectoris, commonly known as angina, is chest pain due to ischemia (a lack of blood, thus a lack of oxygen supply and waste removal) of the heart muscle, generally due to obstruction or spasm of the coronary arteries (the heart's blood vessels). Coronary artery disease, the main cause of angina, is due to atherosclerosis of the coronary arteries There is a weak relationship between severity of pain and degree of oxygen deprivation in the heart muscle (i.e., there can be severe pain with little or no risk of a heart attack, and a heart attack can occur without pain). Worsening angina attacks, sudden-onset angina at rest, and angina lasting more than 15 minutes are symptoms of unstable angina (usually grouped with similar conditions as the acute coronary syndrome). As these may herald myocardial infarction (a heart attack), they require urgent medical attention and are generally treated as a presumed heart attack.
Angina is chest discomfort that occurs when there is decreased blood oxygen supply to an area of the heart muscle. In most cases, the lack of blood supply is due to a narrowing of the coronary arteries as a result of arteriosclerosis.
Angina is usually felt as:
pressure,
heaviness,
tightening, squeezing, or
Aching across the chest, particularly behind the breastbone.
This pain often radiates to the neck, jaw, arms, back, or even the teeth.
Patients may also suffer:
indigestion,
heartburn,
weakness,
sweating,
nausea,
cramping, and
Shortness of breath.
Angina usually occurs during exertion, severe emotional stress, or after a heavy meal, when the heart muscle demands more blood oxygen than the narrowed coronary arteries can deliver. Angina typically lasts from 1 to 15 minutes and is relieved by rest or by placing a nitroglycerin tablet under the tongue, which relaxes the blood vessels and lowers blood pressure. Both rest and nitroglycerin decrease the heart muscles demand for oxygen, relieving angina
1. Stable angina
2. Unstable angina
3. Microvascular angina
Stable angina is the most common type of angina, and what most people mean when they refer to angina. People with stable angina have angina symptoms on a regular basis and the symptoms are somewhat predictable (for example, walking up a flight of steps causes’ chest pain). For most patients, symptoms occur during exertion and commonly last less than five minutes. They are relieved by rest or medication, such as nitroglycerin under the tongue. Stable angina is one of many causes of chronic chest pain.
Unstable angina is less common but more serious. The symptoms are more severe and less predictable than the pattern of stable angina. Pain is more frequent, lasts longer, occurs at rest, and is not relieved by nitroglycerin under the tongue (or the patient needs to use more nitroglycerin than usual). Unstable angina is not the same as a heart attack, but warrants an immediate visit to your physician or hospital emergency department as further cardiac testing is urgently needed. Unstable angina is often a precursor to a heart attack.
Microvascular Angina or Angina Syndrome X is characterized by angina-like chest pain, but has different causes. The cause of Microvascular Angina is unknown, but it appears to be the result of poor function in the tiny blood vessels of the heart, arms and legs. Since Microvascular angina isn't characterized by arterial blockages, it's harder to recognize and diagnose, but its prognosis is excellent.
Age (≥ 55 years for men, ≥ 65 for women)
Cigarette smoking
Diabetes mellitus (DM)
Dyslipidemia
Family History of premature Cardiovascular Disease (men <55 years, female <65 years old)
Hypertension (HTN)
Kidney disease (microalbuminuria or GFR<60 mL/min)
Obesity (BMI ≥ 30 kg/m2)
Physical inactivity
Medications
vasodilators
excessive thyroid replacement
vasoconstrictors
polycythemia which thickens the blood causing it to slow its flow through the heart muscle
One study found that smokers with coronary artery disease had a significantly increased level of sympathetic nerve activity when compared to those without. This is in addition to increases in blood pressure, heart rate and peripheral vascular resistance associated with nicotine which may lead to recurrent angina attacks. Additionally, CDC reports that the risk of CHD (Coronary heart disease), stroke, and PVD (Peripheral vascular disease) is reduced within 1–2 years of smoking cessation. In another study, it was found that after one year, the prevalence of angina in smoking men under 60 after an initial attack was 40% less in those who had quit smoking compared to those who continued. Studies have found that there are short term and long term benefits to smoking cessation.
profound anemia
uncontrolled HTN
hyperthyroidism
hypoxemia
tachyarrhythmia
bradyarrhythmia
valvular heart disease
hypertrophic cardiomyopathy
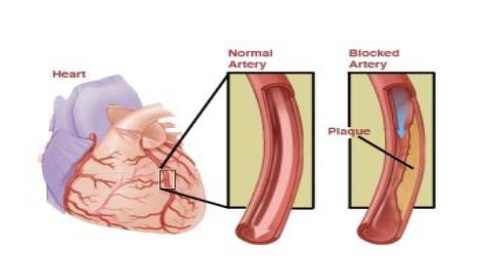
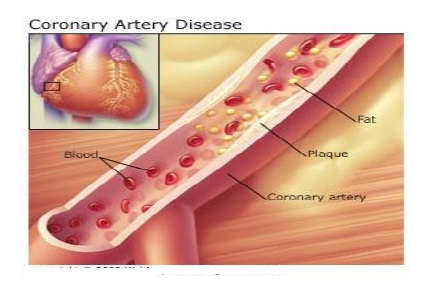
Coronary arteries supply oxygenated blood to the heart muscle. Coronary artery disease develops as cholesterol is deposited in the artery wall, causing the formation of a hard, thick substance called cholesterol plaque. The accumulation of cholesterol plaque over time causes narrowing of the coronary arteries, a process called arteriosclerosis. Arteriosclerosis can be accelerated by smoking, high blood pressure, elevated cholesterol, and diabetes. When coronary arteries become narrowed by more than 50% to 70%, they may no longer be able to meet the increased blood oxygen demand by the heart muscle during exercise or stress. Lack of oxygen to the heart muscle causes chest pain (angina)
Angina is usually a warning sign of the presence of significant coronary artery disease. Patients with angina are at risk of developing a heart attack (myocardial infarction). A heart attack is the death of heart muscle precipitated by the complete blockage of a diseased coronary artery by a blood clot.
During angina, the lack of oxygen (ischemia) to the heart muscle is temporary and reversible. The lack of oxygen to the heart muscle resolves and the chest pain disappears when the patient rests or takes nitroglycerin. In contrast, the muscle damage in a heart attack may be permanent, if there is a delay in obtaining emergency treatment. The dead muscle turns into scar tissue when healed. A scarred heart that results from a heart attack cannot pump blood as efficiently as a normal heart, and can lead to heart failure. Many patients with significant coronary artery disease have no symptoms at all, even though they clearly lack adequate blood and oxygen supply to the heart muscle. These patients have "silent" angina. They have the same risk of heart attack as those with symptoms of angina.
The electrocardiogram (EKG or ECG) is a recording of the electrical activity of the heart muscle, and can detect heart muscle which is in need of oxygen. The EKG is useful in showing changes caused by inadequate oxygenation of the heart muscle or a heart attack.
In patients with a normal resting EKG, exercise treadmill or bicycle testing can be useful screening tools for coronary artery disease. During an exercise stress test (also referred to as stress test, exercise electrocardiogram, graded exercise treadmill test, or stress ECG), EKG recordings of the heart are performed continuously as the patient walks on a treadmill or pedals on a stationary bike at increasing levels of difficulty. The occurrence of chest pain during exercise can be correlated with changes on the EKG, which demonstrates the lack of oxygen to the heart muscle.
When the patient rests, the angina and the changes on the EKG which indicate lack of oxygen to the heart can both disappear. The accuracy of exercise stress tests in the diagnosis of significant coronary artery disease is 60% to 70%. If the exercise stress test does not show signs of coronary artery disease, a nuclear agent (thallium or cardiolyte) can be given intravenously during the test. The addition of thallium or cardiolyte allows nuclear imaging of blood flow to different regions of the heart, using an external camera. A reduced blood flow in an area of the heart during exercise, with normal blood flow to the area at rest, signifies significant artery narrowing in that region of the heart.
Stress echocardiography combines echocardiography (ultrasound imaging of the heart muscle) with exercise stress testing. Like the exercise thallium test, stress echocardiography is more accurate than an exercise stress test in detecting coronary artery disease. When a coronary artery is significantly narrowed, the heart muscle supplied by this artery does not contract as well as the rest of the heart muscle during exercise. Abnormalities in muscle contraction can be detected by echocardiography. Stress echocardiography and thallium stress tests are both about 85% to 90% accurate in detecting significant coronary artery disease. When a patient cannot undergo exercise stress test because of neurological or orthopedic difficulties, medications can be injected intravenously to simulate the stress on the heart normally brought on by exercise. Heart imaging can be performed with a nuclear camera or echocardiography.
Cardiac catheterization with angiography (coronary arteriography) is a technique that allows X-ray pictures to be taken of the coronary arteries. It is the most accurate test to detect coronary artery narrowing. Small hollow plastic tubes (catheters) are advanced under X-ray guidance to the openings of the coronary arteries. Iodine contrast "dye" is injected into the arteries while an X-ray video is recorded. Coronary arteriography gives the doctor a picture of the location and severity of coronary artery disease. This information can be important in helping doctors’ select treatment options.
CT coronary angiography is procedure that uses an intravenous dye that contains iodine, and CT scanning to image the coronary arteries. While the use of catheters is not necessary (this procedure is considered "noninvasive"), there are still some risks involved, including: patients allergic to iodine; patients with abnormal kidney function; and Radiation exposure which is similar to, or greater than, that received with a conventional coronary angiogram.
The most specific medicine to treat angina is nitroglycerin. It is a potent vasodilator that makes more oxygen available to the heart muscle. Beta-blockers and calcium channel blockers act to decrease the heart's workload, and thus its requirement for oxygen. Nitroglycerin should not be given if certain inhibitors such as Sildenafil (Viagra), Tadalafil (Cialis), or Vardenafil (Levitra) have been taken within the previous 12 hours as the combination of the two could cause a serious drop in blood pressure. Treatments are balloon angioplasty, in which the balloon is inserted at the end of a catheter and inflated to widen the arterial lumen. Stents to maintain the arterial widening are often used at the same time. Surgery involves bypassing constricted arteries with venous grafts. This is much more invasive than angioplasty.
The main goals of treatment in angina pectoris are relief of symptoms, slowing progression of the disease, and reduction of future events, especially heart attacks and, of course, death. Beta blockers (e.g., carvedilol, propranolol, atenolol) have a large body of evidence in morbidity and mortality benefits (fewer symptoms, less disability and longer life) and short-acting nitroglycerin medications have been used since 1879 for symptomatic relief of angina. Calcium channel blockers (such as nifedipine (Adalat) and amlodipine), isosorbide mononitrate and nicorandil are vasodilators commonly used in chronic stable angina. A new therapeutic class, called if inhibitor, has recently been made available: ivabradine provides pure heart rate reduction leading to major anti-ischemic and antianginal efficacy.
ACE inhibitors are also vasodilators with both symptomatic and prognostic benefit and, lastly, statinsare the most frequently used lipid/cholesterol modifiers which probably also stabilize existing atheromatous plaque[.Low-dose aspirin decreases the risk of heart attack in patients with chronic stable angina, and was previously part of standard treatment; however, it has since been discovered that the increase in haemorrhagic stroke and gastrointestinal bleeding offsets this gain so they are no longer advised unless the risk of myocardial infarction is very high. Exercise is also a very good long term treatment for the angina (but only particular regimens - gentle and sustained exercise rather than intense short bursts), probably working by complex mechanisms such as improving blood pressure and promoting coronary artery collateralisation.
Angina pectoris is a chest pain caused by decrease oxygen supply to the heart muscle .ECG ,stress test and blood test are important in the diagnosis of angina .It is managed with rest, medication and surgery.
www.google.com
www.wikipedia.com
www.medscape.com
www.emedicinehealth.com
www.medicinenet.com
Angina pectoris by Alice Gallo, Margaret L. Jones